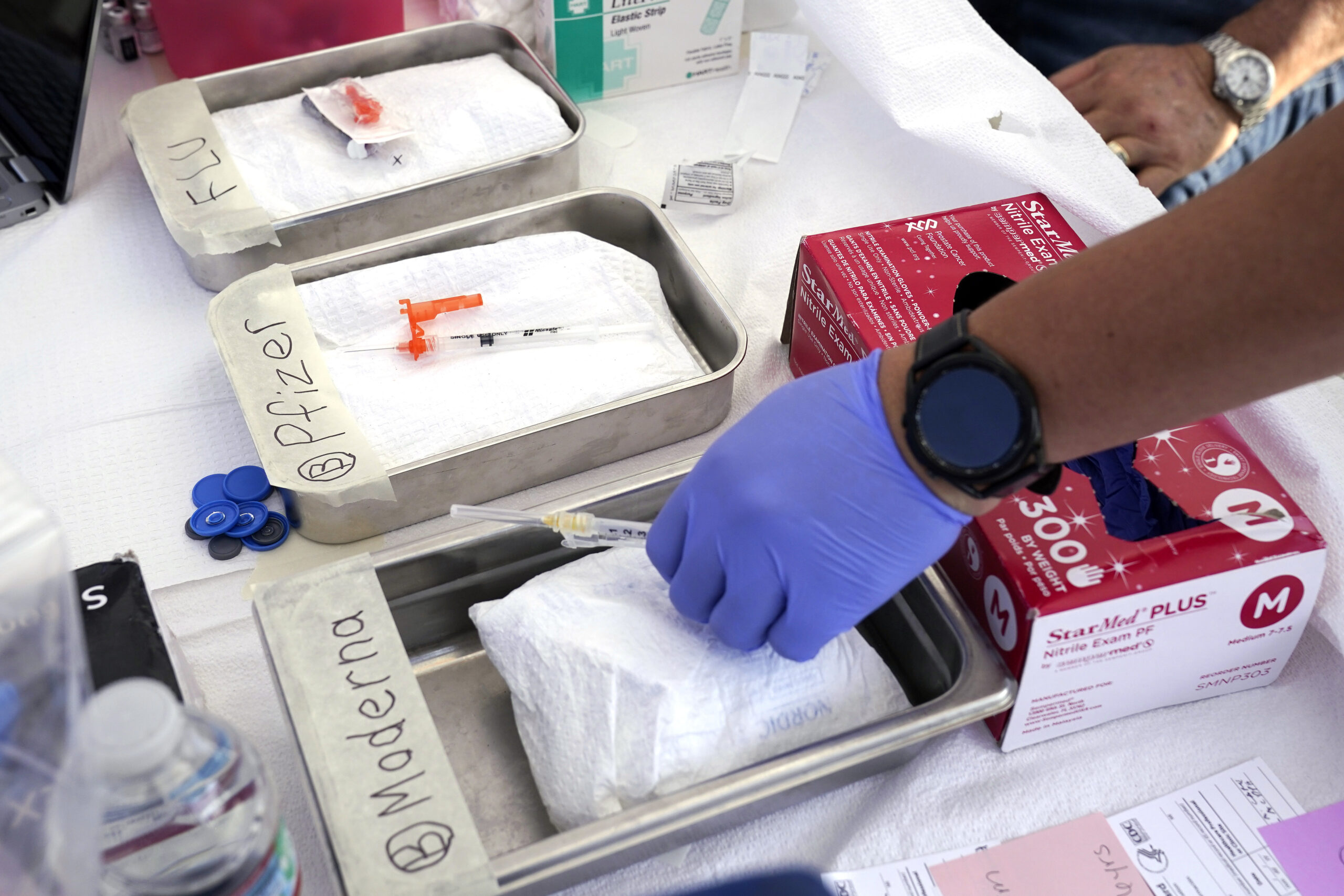
The beginning of the Covid vaccine distribution has been difficult.
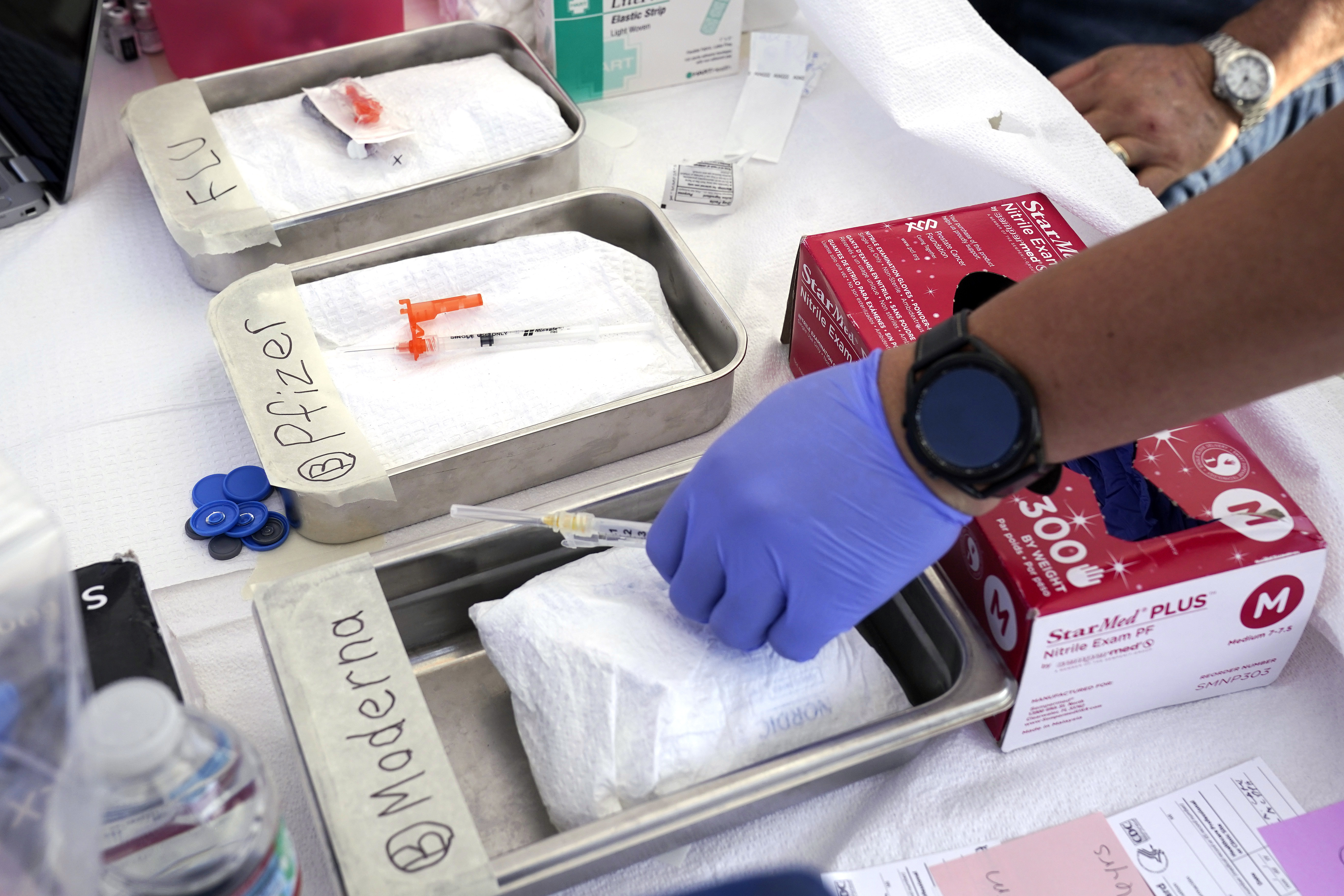
The latest release of Covid-19 vaccines has encountered obstacles due to the discontinuation of the federal government’s procurement and distribution of the doses.
Most Americans with public and private health insurance can still get the shot for free, as long as they visit in-network providers. But as the vaccines make their debut on the commercial market, a mix of distribution hiccups and confusion over insurance coverage has led people to walk out of pharmacies without their Covid shot.
In certain scenarios, pharmacies may not have any available vaccinations; while in others, individuals are being requested to pay hundreds of dollars for a service they believed would be covered by their insurance.
The initial challenges pose a potential problem for the government’s goal of widespread adoption of the latest vaccine and a better success rate than last year’s vaccine, which was only received by around 17% of the U.S., according to CDC data from May. Health professionals are concerned about pandemic fatigue and the increasing resistance to vaccines, which could further discourage Americans from getting this shot if the rollout is problematic.
The American Pharmacists Association’s senior vice president for pharmacy practice and government affairs, Ilisa Bernstein, expresses concern that patients who are not covered for their vaccine may not return, resulting in a missed opportunity.
Even though the country is not currently experiencing a pandemic, there has been a gradual increase in the number of COVID cases and hospitalizations over the past few months. The Biden administration is worried about the situation and has decided to relaunch its mail-order COVID testing program this week.
Initial issues led to accusations over who is accountable: Insurers accused pharmacists of incorrectly coding the vaccines, while pharmacists blamed suppliers for inadequate delivery of shots.
The reported issues and confusion experienced nationwide were downplayed, with pharmacies working to resolve them. On Wednesday, it was emphasized to individuals to reach out to their insurance providers if they faced any difficulties.
Representatives from Humana, Cigna, Blue Cross Blue Shield, and Elevance Health informed POLITICO that the majority of their members are eligible to receive the vaccine without any cost. According to a spokesperson from Cigna Healthcare, the company recently revised their codes and there have been instances of incorrect claim submissions by certain pharmacies.
There was no response from United when asked for a comment.
According to a statement from America’s Health Insurance Plans, their members are providing coverage for Covid-19 vaccinations when received from in-network providers.
The organization stated that they are collaborating with the federal government, pharmacies, and other partners to promptly provide patients with COVID-19 vaccines at no cost. They are also addressing any concerns regarding newly added billing codes in a timely manner.
According to Kates, individuals with insurance may still incur costs not covered by their plan if they receive care from a provider outside of their network. This may not apply if there are no providers within the network who offer the necessary treatment.
In the meantime, pharmacies anticipate that the majority of problems will be promptly addressed.
According to Rite Aid representative Catherine Carter, the company has not encountered any coding or billing difficulties with the latest vaccines. These vaccines are anticipated to be available in stores by the upcoming weekend, although there have been instances where there is a limited supply of shots.
In a statement, she explained that the demand for the new COVID-19 vaccine has surpassed the supply provided by the manufacturer in numerous stores.
According to Walgreens representative Erin Loverher, the majority of the company’s stores have an adequate supply of doses to accommodate current appointments. However, there have been some instances of supply delays at certain locations, causing a temporary pause in online scheduling.
According to CVS spokesperson Matt Blanchette, the new shots are being delivered to stores gradually and some appointments may need to be rescheduled due to delays in delivery to certain locations.
According to pharmacists interviewed by POLITICO, they anticipate that the supply and coverage problems will improve in the next few weeks as more vaccines are distributed to providers and as insurance companies and pharmacies update their processes.
Last week, the FDA and CDC gave their approval for the Pfizer and Moderna vaccines, which have been modified to target the specific Covid variant that was prevalent during late spring and early summer. Once CDC Director Mandy Cohen officially recommended the vaccines, manufacturers started distributing doses.
However, with pharmacies now required to cover the cost of doses in advance, they must carefully consider these expenses in relation to expected demand and potential payment issues from insurers.
Pharmacist Brian Caswell from Baxter Springs, Kansas has not had an opportunity to test certain matters due to the delayed delivery of his Moderna order. He has also noticed advertisements on television stating that the vaccines are accessible at nearby pharmacies.
Caswell told POLITICO that it is ironic because none of his pharmacies, including the one I am currently in, have them.
Representatives from Pfizer and Moderna have stated that they have an ample supply of doses to disperse, as each company has already shipped millions of doses.
After months of preparation within the administration, the initial challenges arose in transitioning to a commercialized system.
Earlier this summer, officials from the Biden administration expressed concerns that the transition could be difficult. A Biden official who was involved in internal discussions, but not allowed to speak on the record, stated that the officials advised leaders from the Department of Health and Human Services (HHS) to collaborate closely with insurance companies and pharmacies to ensure their employees were adequately trained and ready.
In July, CMS issued a notification to insurers, informing them to get ready for the change. In August, the American Medical Association released updated codes for insurers to utilize for the newly approved vaccines. After the vaccines were authorized, CMS sent another notification to insurers containing the new codes. In September, HHS introduced the Bridge Access Program, which offers free vaccinations to those without insurance.
According to Bernstein from APhA, it is not uncommon for there to be conflicts between pharmacy and plan systems when a new medical product is introduced.
“It’s like a perfect combination of multiple events taking place simultaneously,” she stated.
Source: politico.com