No one’s promising you can keep your doctor anymore
President Barack Obama famously assured Americans that they would be able to retain their doctors. However, with the current trends, it is likely that a significant number of Americans will not have a doctor at all, or at least not in the traditional sense.
The equation is straightforward: The number of doctors produced by medical schools is insufficient to match the growing population.
Wealthy individuals will have the option to keep their own doctor through specialized “concierge medicine” offerings. However, those who are not as financially well-off can anticipate regular appointments with different nurses and physician assistants, as well as virtual checkups with doctors. This shift has prompted Congress and the Biden administration to work on creating a primary care system that can accommodate the general population before it becomes difficult to schedule appointments.
“You won’t be returning to the past.”Bernie Sanders
In an interview, the chair of the Senate committee in charge of the country’s healthcare, Senator (I-Vt.), stated.
Both the Republican and Democratic parties are in agreement that the previous approach is no longer possible, and they are actively contributing to its downfall.
Sanders and Kansas Republican Sen. have jointly introduced a bill.Roger Marshall
The purpose of this is to restructure primary healthcare, but their objective is not to bring back the dominance of individual practices where a local doctor cared for a community for many years. Sanders acknowledged that this era has mostly passed.
The number of visits managed by individuals who are not doctors almost doubled from 2013 to 2019.
Many physicians express concern over the effects on patient care, but this change is a result of larger factors. Doctors report that the high costs of overhead and increasing administrative responsibilities make it impossible to maintain a small independent practice. In comparison to other fields of medicine, primary care physicians often work extended hours for less compensation.
According to a recent report from the Primary Care Collaborative, a non-profit organization representing clinicians and healthcare organizations, there is a larger number of primary care doctors retiring or leaving the field compared to new medical school graduates who are pursuing a career in family medicine. Additionally, every state has experienced a decline in the number of primary care doctors per capita.
In order to address this lack, the Biden administration and Congress are promoting policies to alter the way primary care providers are compensated and to incentivize nurses to take on more responsibilities. They are also supporting the growth of virtual care by removing limitations on its utilization.
The government has allocated more than $100 million in funding for the training of additional nurses. This includes a focus on enhancing their education so that they can establish independent primary care practices.
“We are carrying out this action in response to directives given to us,” stated Secretary of Health and Human Services Xavier Becerra during the announcement of the grants. “These directives were given directly by President Biden.”
The situation in the nation’s capital is hastening a pattern that numerous Americans are realizing when searching for a new physician or attempting to schedule an appointment with a previous one. The customary yearly physical, done in person with a doctor, is becoming increasingly difficult to obtain.
Primary care reimagined
A common annoyance for many Americans is when they fall ill, and by the time they can schedule an appointment with their doctor, they have already recovered.
Therefore, individuals frequently visit the emergency room, urgent care clinics, or pharmacy clinics for medical evaluation.
Patients are facing a medical system that is centered on transactions rather than the idealized past, causing them frustration in getting proper attention.
According to Sanders, many people feel that the current system lacks a personal connection between patients and doctors. The doctor is not aware of the patient’s family dynamics or the challenges they may be facing.
Sanders and Marshall are proposing a fresh strategy in which community health centers will cater to a larger population. These centers focus on providing affordable and accessible preventive care, a departure from the traditional approach of physician practices. This will particularly benefit patients with limited or no insurance coverage.
“Sanders expressed that his bill could be considered transformative and a step towards progress.”
The proposed legislation also includes provisions for financing the training of additional healthcare professionals, including doctors, nurses, and advanced nurse practitioners. The goal is to increase the size of the workforce and enhance the skills of those already working within it.
Sanders believes that increasing access to preventive care will ultimately lower expenses, but certain legislators remain unconvinced.
Bill Cassidy, a Republican from Louisiana and a doctor specializing in digestive disorders, is the leading member of Sanders’ committee. He supports the idea of increasing access to community health centers, but he is against the bill due to concerns about its cost.
During the hearing on the proposed legislation, he stated that we may concur with the diagnosis but have differing opinions on the recommended course of action.
Cassidy offered a proposal that would give community health centers a boost in funding, albeit more modest than the one proposed by Sanders and Marshall. But he suggested the private sector should be devising new approaches.
The Biden administration is pursuing a different approach to achieve the same goal – expanding the system to accommodate a larger number of patients.
The Department of Health and Human Services is allocating funds to support primary care physicians, increasing the number of healthcare professionals, and broadening the criteria for what constitutes a primary care provider.
The Centers for Medicare and Medicaid Services intends to increase compensation for medical professionals who offer preventive services, potentially impacting the payment rates for specialists.
The organization is launching a program in eight states with the goal of increasing access to primary care for Medicare and Medicaid recipients over the next ten years. This initiative will work alongside several smaller projects that are currently testing out innovative approaches.
The Department of Veterans Affairs is also involved in the initiative. The organization, responsible for providing healthcare to over 9 million veterans, is working on creating guidelines that would expand the scope of practice for nurses and physician assistants in treating patients.
Several organizations argue that the VA’s choices may significantly influence the standards set by state governments, which are typically responsible for determining regulations.
Take care of the other 50%.
If you are not interested in the new world Congress and the Biden administration, there is another option: concierge medicine.
The catch is that you will have to pay.
Individuals who are willing to cover fees themselves, usually around $2,000 annually, in addition to the already high price of private health insurance, have the ability to schedule appointments with their primary care physicians according to their preferences.
Dr. Elisabeth Wilson, a family physician who leads the community and family medicine department at Dartmouth Health and the Geisel School of Medicine in New Hampshire, explained that obtaining this care takes resources. This may prevent individuals who are financially struggling, uninsured, or relying on public insurance from being able to receive the necessary care.
Concierge medicine is attractive because it eliminates the need for patients to schedule appointments far in advance. There is no wait time, appointments are not rushed, and doctors are available for phone calls. In some cases, concierge doctors may even accompany patients during visits with specialists to offer input on their care.
MDVIP, the biggest concierge group in the country, has 1,200 doctors who are affiliated with them and treat a total of 385,000 patients. According to their estimates, there are approximately 6,500 concierge providers in the field overall.
This represents only a small portion of the country’s estimated 200,000 doctors who specialize in family and internal medicine on a full-time basis.
However, the popularity of concierge medicine is increasing consistently. A recent report from a market research company estimates that the growth rate will be over 10% annually between now and 2030.
Major technology companies are attempting to lower the cost of membership-based primary care, but without guaranteeing a personal connection with a physician.
In the beginning of this month, Amazon declared that individuals with a Prime membership ($14.99 per month) can add $9 every month to become a part of its One Medical division, which grants them access to 24/7 virtual medical services and convenient scheduling for in-person appointments.
The company is meeting strong consumer demand.
According to Dr. Sunita Mishra, chief medical officer of Amazon Health Services, consumers desire round-the-clock access to their doctor, but it is not feasible for the doctor to be physically present at all times.
The appointment is ready for you to be seen.
Recent checks of insurance companies’ lists of primary care providers reveal that a significant number are not doctors, but rather nurses or physician assistants.
This is a characteristic of the updated primary care system, not a flaw. Broadening the responsibilities of nurses and physician assistants is one strategy that policymakers are utilizing to enhance access to healthcare.
Both the Biden and Trump administrations have provided funding for nurse practitioner residency programs, with the goal of allowing NPs to take on tasks that were previously only done by doctors.
The changes have been historically opposed by groups of doctors, and many continue to do so. Their argument is that it will put patients at risk and ultimately lead to higher costs for healthcare.
Dr. Gary Floyd, a former president of the Texas Medical Association, stated to POLITICO that what is necessary is implementing initiatives that will boost the amount of physicians in our healthcare system. This statement came after the Biden administration revealed plans to provide grants for nurse practitioners to establish their own practices.
Nurse practitioner organizations have stated that they possess sufficient training to assume a greater responsibility in the system, and that antiquated laws must be revised to reflect this.
Numerous primary care physicians have recognized the need for a shift in the system and have willingly delegated more of their responsibilities. By entrusting tasks to nurses and physician assistants, they are able to see more patients and potentially increase their earnings.
The reason for its effectiveness is attributed to the continual supervision of a physician.
Wilson, a family physician in New Hampshire, expressed excitement about the increase in nurse practitioners and physician assistants. She emphasized the importance of educating people about the benefits of a collaborative healthcare approach, which ultimately leads to improved care and outcomes for patients.
Dr. Ateev Mehrotra, a professor of health care policy and medicine at Harvard Medical School, oversaw the BMJ study that found a rapid increase starting a decade ago in patient visits handled by non-doctors.
According to him, the study implies that nurse practitioners may be treating milder illnesses such as urinary tract infections, respiratory illnesses, and annual check-ups, rather than replacing doctors. In turn, doctors can focus on more critical cases such as heart disease and initial visits from new patients.
Mehrotra stated that while it is occurring, it is uncertain whether it is resulting in improved or worsened care. They are not aware of any evidence that should cause concern for the general public.
A tech transformation
During the Covid pandemic, the use of telehealth significantly increased due to the Trump administration and Congress allowing Medicare to cover virtual appointments.
Lawmakers have approved the extension of those authorizations until 2024 and are currently considering making them permanent.
In the business world, there was a significant increase in investment for virtual healthcare services.
Initial studies have shown that expanded virtual healthcare has been mostly favorable, revealing that individuals who are able to easily access healthcare are more inclined to seek it out. Additionally, receiving routine preventative care can contribute to better long-term health.
However, this also implies decreased in-person interaction with a specific physician. Telehealth models usually assign patients to various available healthcare professionals, including doctors, nurses, and physician assistants.
Certain telehealth companies are testing out strategies that aim to maintain the compassionate aspect of healthcare.
Mehrotra highlighted Iora Health as an example. This healthcare organization utilizes health coaches as the main connection for patients, while doctors oversee treatment behind the scenes. The goal is to provide culturally sensitive care by hiring coaches from the patient’s community, and in some cases, their hometown.
Iora was acquired by One Medical in 2021 and is now a subsidiary of Amazon.
Some other companies, such as Firefly Health, view a virtual care approach as a means to provide patients with a wider range of providers who are specialized in their specific needs or with whom they have a stronger connection.
According to Wilson, virtual appointments are beneficial for her patients who live in rural areas as it saves them from long drives and missing work. She believes it is a convenient way to monitor chronic illnesses or discuss the potential drawbacks of a new medicine.
However, she is concerned about potentially losing an important aspect of what primary care physicians enjoy about their profession: building relationships.
She mentioned the importance of face-to-face communication.
Farewell to the primary care physician.
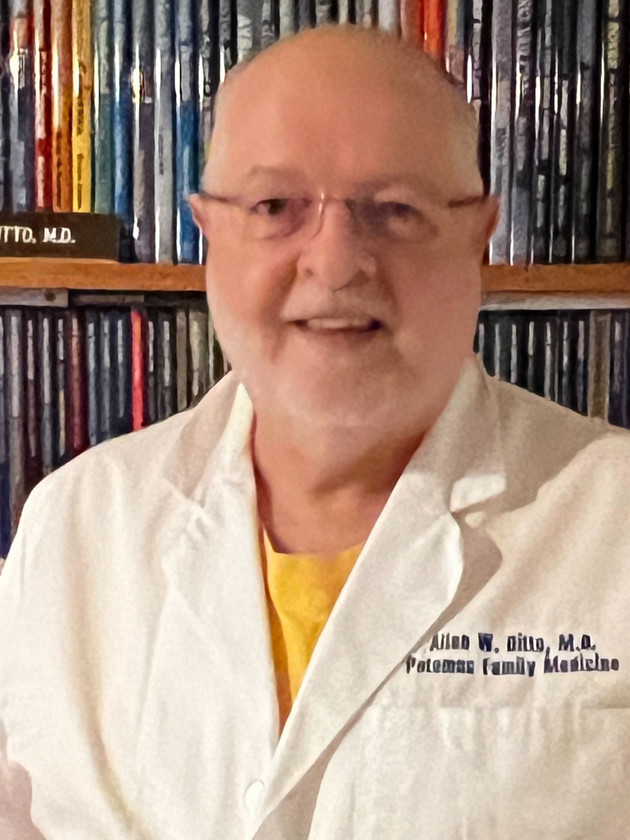
Dr. Allen Ditto is one of the few remaining individuals of a diminishing type.
He is a third-generation primary care physician who was raised accompanying his father and grandfather on house calls.
During his nearly four-decade tenure in Hagerstown, Maryland, a small town 70 miles northwest of Washington, Ditto’s independent practice became unmanageable. He transitioned from working on his own to joining a group practice and eventually became part of a local health system before retiring in 2019. In the later years of his career, he was approached by a concierge medical company, but ultimately chose not to make the switch.
He stated that it is no longer feasible to work independently and that the bureaucratic processes required by insurance companies are both time-consuming and overwhelming. He believes that this is hindering progress and finds the system unnecessarily convoluted.
According to Wilson, the additional administrative tasks after regular work hours have influenced younger colleagues to opt out of full-time clinical care. She mentioned that they are aware that their evenings and weekends will be occupied.
However, she remains optimistic about the field and views family medicine as a social movement that can address the healthcare needs of our communities. She stated, “It offers a means to offer the necessary care to our communities.”
The appearance of that concern is now distinct from what it used to be. According to her, smaller practices with just one or two employees can no longer sustain their operations.
Ditto’s offspring is also a medical professional, but has opted for a different career path from his father. He works part-time and also educates residents in family medicine at the nearby hospital system.
Source: politico.com