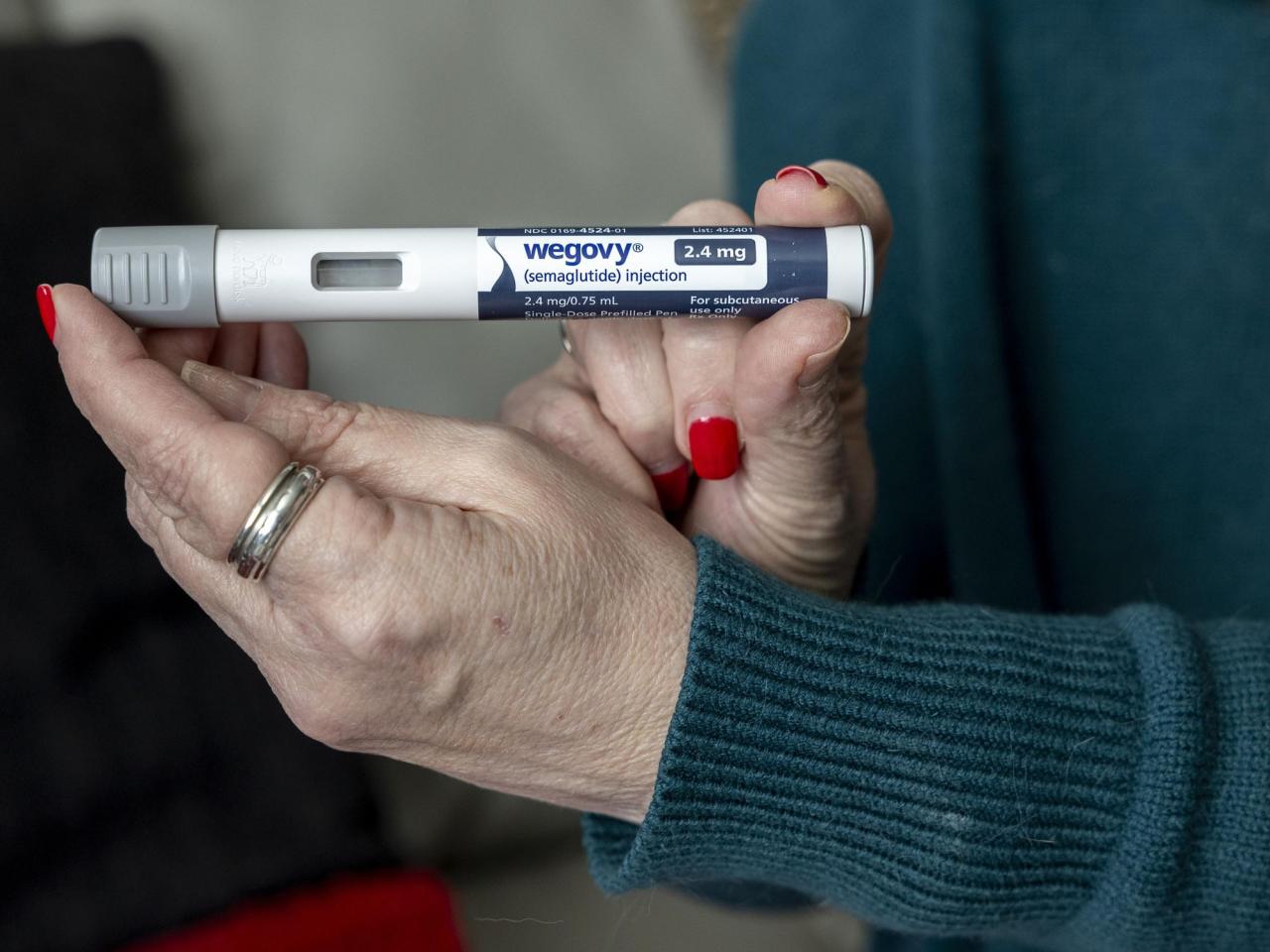
In specific heart patients, Medicare is able to cover the cost of weight loss medications, such as Wegovy.
On Thursday, federal officials announced that Medicare can cover the cost of the widely-used weight loss medication Wegovy, but only for patients who also have heart disease and require it to lower the likelihood of future heart attacks, strokes, and other severe issues.
The Centers for Medicare & Medicaid Services have released updated instructions stating that Medicare Part D drug benefit plans, provided by private insurers, may now cover anti-obesity medications that have been approved for alternative purposes.
Analysts have stated that this decision could lead to a significant increase in spending, potentially resulting in billions of dollars in new prescriptions being filled.
The new guidelines make it possible for Wegovy, a medication for obesity made by Novo Nordisk, to have a broader scope of coverage. This is thanks to a recent label change approved by the U.S. Food and Drug Administration that now permits Wegovy to be prescribed for individuals who are overweight or have obesity and also have preexisting heart conditions in order to decrease the risk of cardiovascular problems.
New studies revealed that Wegovy lowered the chances of suffering a heart attack, stroke, or other related issues by 20% compared to a fake drug, in patients with these conditions. Specialists in heart health stated that utilizing semaglutide to decrease the risk of severe and debilitating conditions could have a significant impact on the treatment of heart patients.
Wegovy costs over $1,300 per month, or $16,000 per year.
According to Tricia Neuman, a Medicare specialist at KFF, a non-profit organization focused on health policy research, Part D plans may start providing coverage for the medication within the current year.
According to her, Medicare plans may hesitate to swiftly expand coverage for WeGovy due to its comparatively expensive cost. This is because they will not have the ability to modify premiums until next year.
Even if individuals qualify for coverage, they may still encounter limitations such as increased out-of-pocket costs, prior approval, or step therapy, according to Neuman. This means the patient may be required to try a less expensive medication before they can access the prescribed treatment.
According to CMS officials, Medicare Part D plans are not allowed to include coverage for obesity medications solely for chronic weight management purposes and this is not subject to change by law.
Private insurance providers are currently reviewing the recommendations and updating their coverage policies in regards to Wegovy’s new purpose, as mentioned by a representative from AHIP (America’s Health Insurance Plans), a trade association for the insurance industry.
___
Pharmaceutical companies and supporters of fighting obesity have been advocating for increased insurance coverage, including proposed laws that would mandate Medicare to cover the cost of medications for obesity.
The debate is centered around whether the high cost of medication will be balanced out by the decrease in expenses for healthcare related to obesity and heart disease.
The FDA reports that the limited availability of the drug has been hindering its widespread use for over a year. In response, representatives from Novo Nordisk state that they are actively working to improve production and availability.
___
The AP Health and Science Department is backed by the Science and Educational Media Group of the Howard Hughes Medical Institute. The AP is fully accountable for all material.