A twice-yearly shot could help end AIDS. But will it get to everyone who needs it?
MEXICO CITY (AP) — It’s been called the closest the world has ever come to a vaccine against the AIDS virus.
The twice-yearly shot was 100% effective in preventing HIV infections in a study of women, and results published Wednesday show it worked nearly as well in men.
Drugmaker Gilead said it will allow cheap, generic versions to be sold in 120 poor countries with high HIV rates — mostly in Africa, Southeast Asia and the Caribbean. But it has excluded nearly all of Latin America, where rates are far lower but increasing, sparking concern the world is missing a critical opportunity to stop the disease.
“This is so far superior to any other prevention method we have, that it’s unprecedented,” said Winnie Byanyima, executive director of UNAIDS. She credited Gilead for developing the drug, but said the world’s ability to stop AIDS hinges on its use in at-risk countries.
In a report issued to mark World AIDS Day on Sunday, UNAIDS said that the number of AIDS death last year — an estimated 630,000 — was at its lowest since peaking in 2004, suggesting the world is now at “a historic crossroads” and has a chance to end the epidemic.
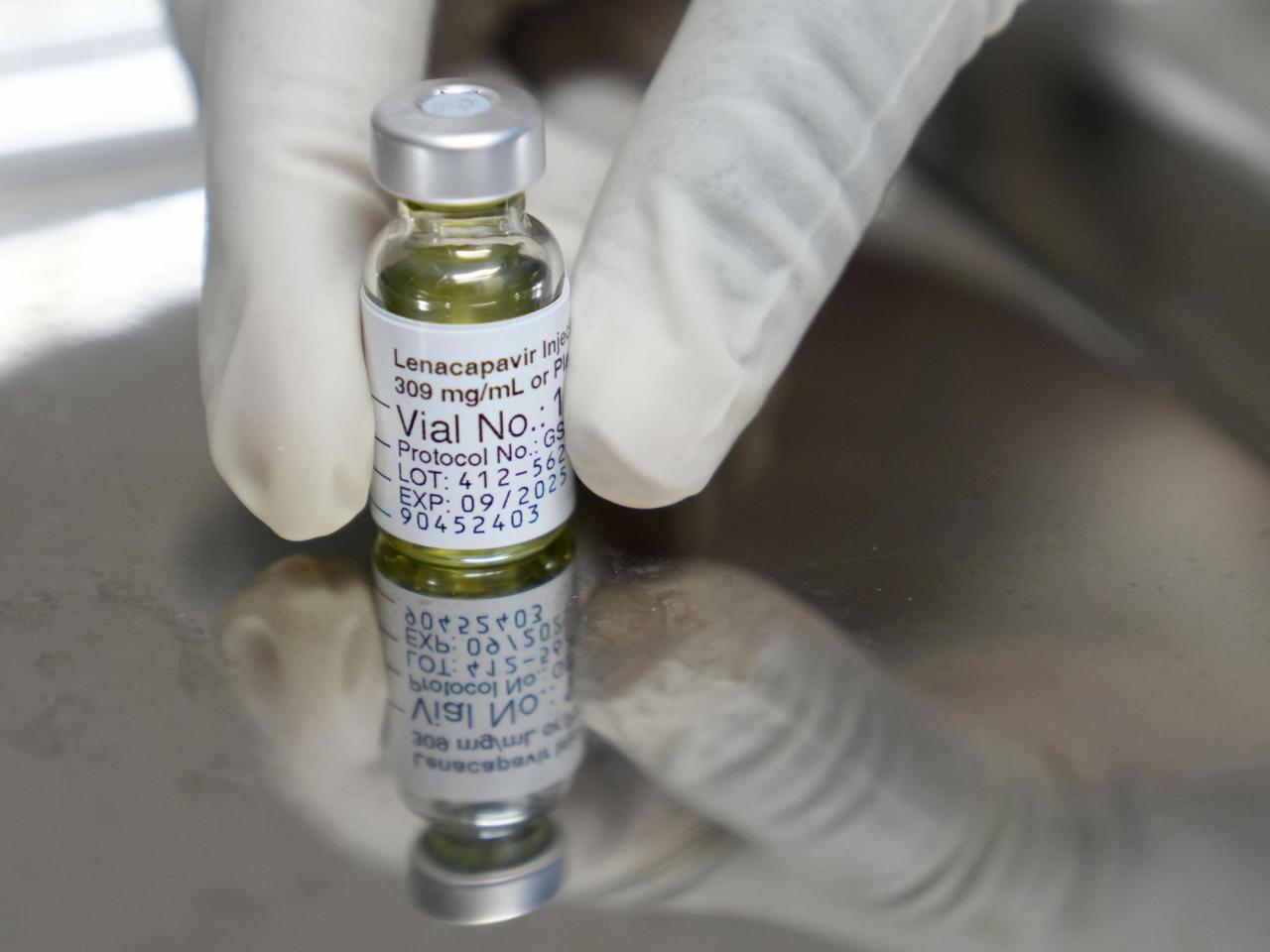
The drug called lenacapavir is already sold under the brand name Sunlenca to treat HIV infections in the U.S., Canada, Europe and elsewhere. The company plans to seek authorization soon for Sunlenca to be used for HIV prevention.
While there are other ways to guard against infection, like condoms, daily pills, vaginal rings and bi-monthly shots, experts say the Gilead twice-yearly shots would be particularly useful for marginalized people often fearful of seeking care, including gay men, sex workers and young women.
“It would be a miracle for these groups because it means they just have to show up twice a year at a clinic and then they’re protected,” said UNAIDS’ Byanyima.
Such was the case for Luis Ruvalcaba, a 32-year-old man in Guadalajara, Mexico, who participated in the latest published study. He said he was afraid to ask for the daily prevention pills provided by the government, fearing he would be discriminated against as a gay man. Because he took part in the study, he’ll continue to receive the shots for at least another year.
“In Latin American countries, there is still a lot of stigma, patients are ashamed to ask for the pills,” said Dr. Alma Minerva Pérez, who recruited and enrolled a dozen study volunteers at a private research center in Guadalajara.
How widely available the shots will be in Mexico through the country’s health care system isn’t yet known. Health officials declined to comment on any plans to buy Sunlenca for its citizens; daily pills to prevent HIV were made freely available via the country’s public health system in 2021.
“If the possibility of using generics has opened, I have faith that Mexico can join,” said Pérez.
Byanyima said other countries besides Mexico that took part in the research were also excluded from the generics deal, including Brazil, Peru and Argentina. “To now deny them that drug is unconscionable.” she said.
In a statement, Gilead said it has “an ongoing commitment to helping enable access to HIV prevention and treatment options where the need is the greatest.” Among the 120 countries eligible for generic version are 18 mostly African countries that comprise 70% of the world’s HIV burden.
The drugmaker said it is also working on establishing “fast, efficient pathways to reach all people who need or want lenacapavir for HIV prevention.”
On Thursday, 15 advocacy groups in Peru, Argentina, Ecuador, Chile, Guatemala and Colombia wrote to Gilead, asking for generic Sunlenca to be made available in Latin America, citing the “alarming” inequity in access to new HIV prevention tools while infection rates were rising.
While countries including Norway, France, Spain and the U.S. have paid more than $40,000 per year for Sunlenca, experts have calculated it could be produced for as little as $40 per treatment once generic production expands to cover 10 million people.
Dr. Chris Beyrer, director of the Global Health Institute at Duke University, said it will be enormously useful to have Sunlenca available in the hardest-hit countries in Africa and Asia. But he said the rising HIV rates among groups including gay men and transgender populations constituted “a public health emergency” in Latin America.
Hannya Danielle Torres, a 30-year-old trans woman and artist who was in the Sunlenca study in Mexico, said she hoped the government would find a way to provide the shots. “Mexico may have some of the richest people in the world but it also has some of the most vulnerable people living in extreme poverty and violence,” Torres said.
Another drugmaker, Viiv Healthcare, also left out most of Latin America when it allowed generics of its HIV prevention shot in about 90 countries. Sold as Apretude, the bi-monthly shots are about 80% to 90% effective in preventing HIV. They cost about $1,500 a year in middle-income countries, beyond what most can afford to pay.
Asia Russell, executive director of the advocacy group Health Gap, said that with more than 1 million new HIV infections globally every year, established prevention methods are not enough. She urged countries like Brazil and Mexico to issue “compulsory licenses,” a mechanism where countries suspend patents in a health crisis.
It’s a strategy some countries embraced for previous HIV treatments, including in the late 1990s and 2000s when AIDS drugs were first discovered. More recently, Colombia issued its first-ever compulsory license for the key HIV treatment Tivicay in April, without permission from its drugmaker, Viiv.
Dr. Salim Abdool Karim, an AIDS expert at South Africa’s University of KwaZulu-Natal, said he had never seen a drug that appeared to be as effective as Sunlenca in preventing HIV.
“The missing piece in the puzzle now is how we get it to everyone who needs it,” he said.
___
Cheng reported from London.
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.